Las vacunas son seguras y efectivas. Conozca los hechos.
Las vacunas son una forma extremadamente segura y eficaz de prevenir enfermedades al inmunizar a las personas para protegerlas de enfermedades infecciosas potencialmente mortales como el sarampión, las paperas y la tos ferina.
Las vacunas evitaron millones de muertes por enfermedades infecciosas.


Los beneficios significativos de vacunarse
Victorias históricas sobre la enfermedad
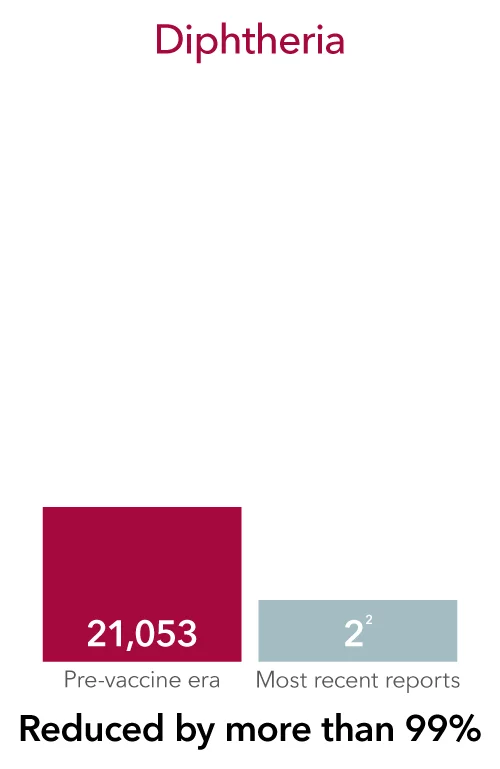
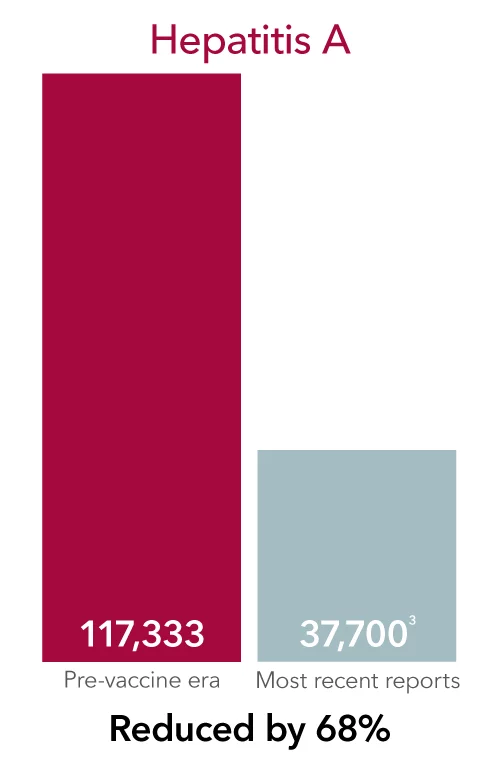
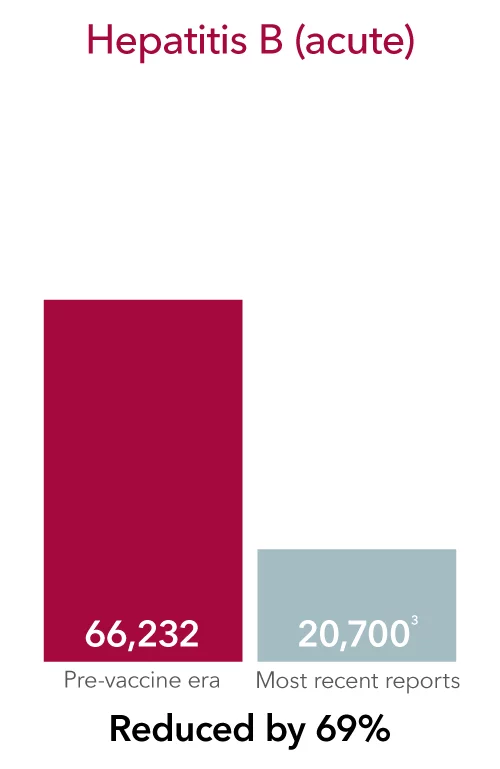
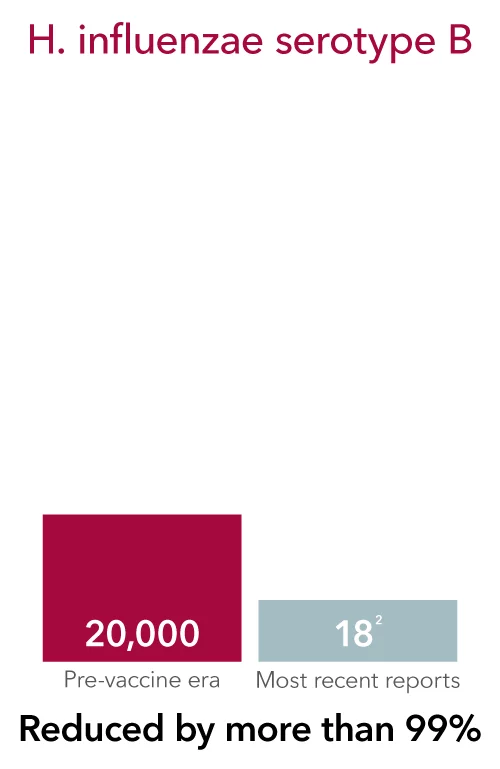
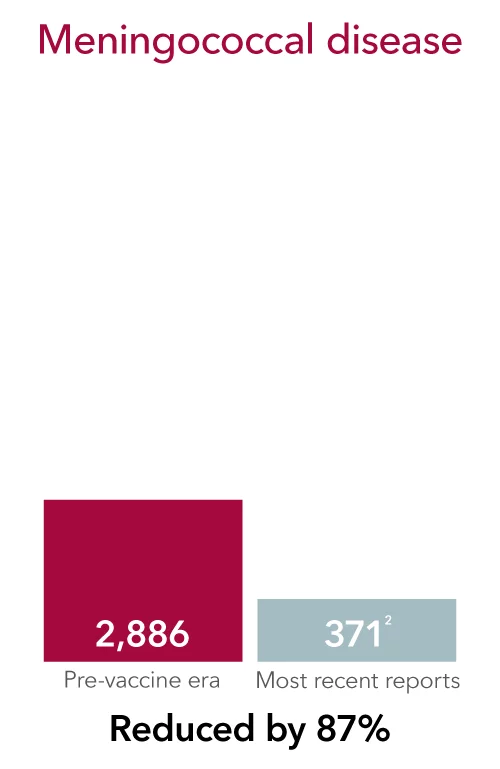
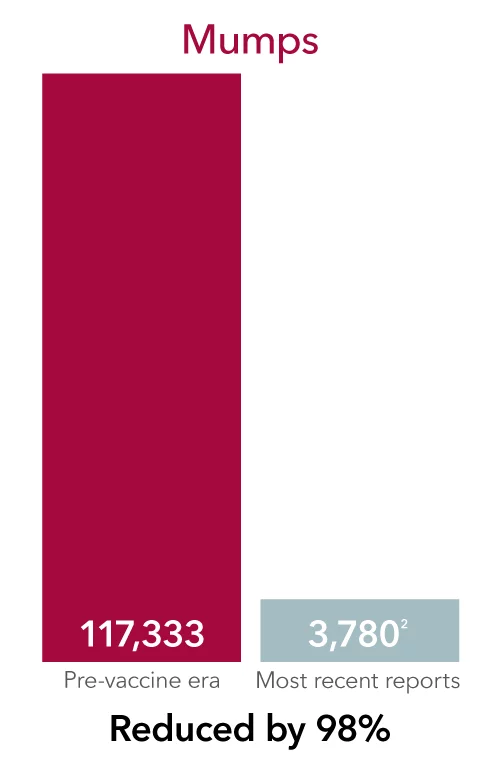
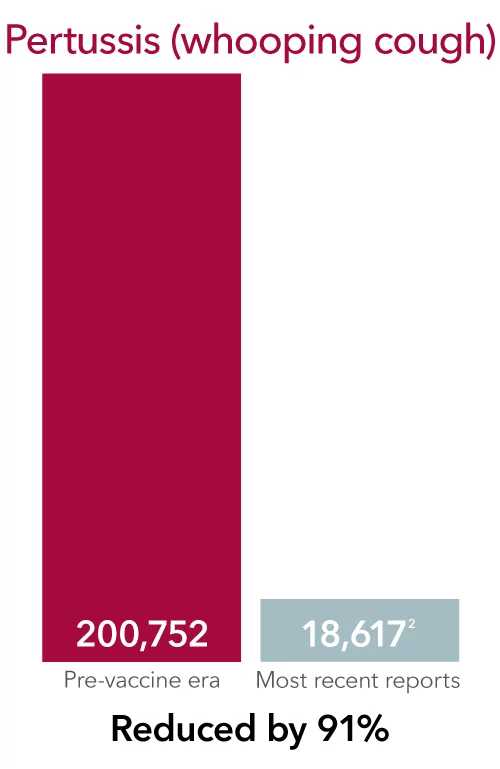
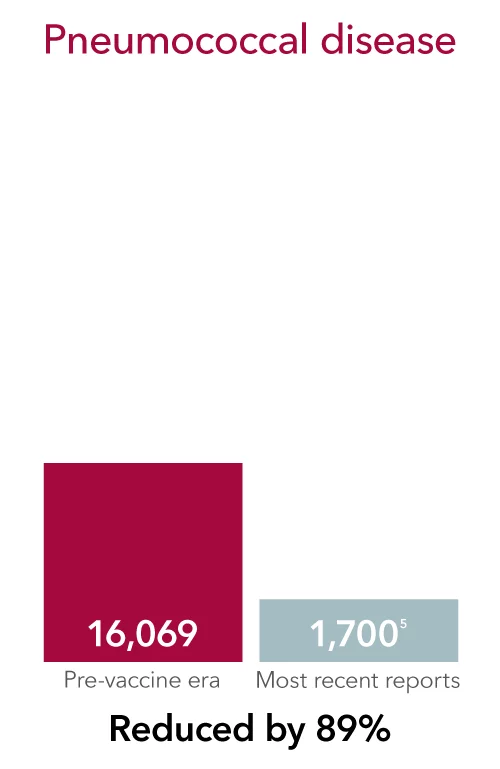
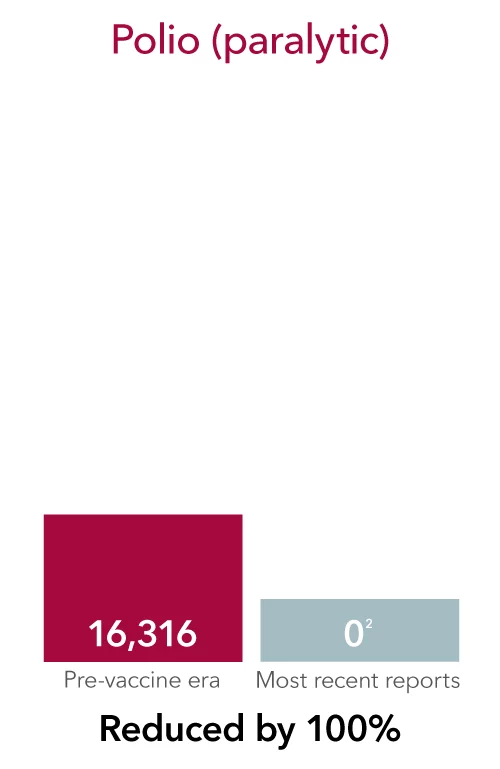
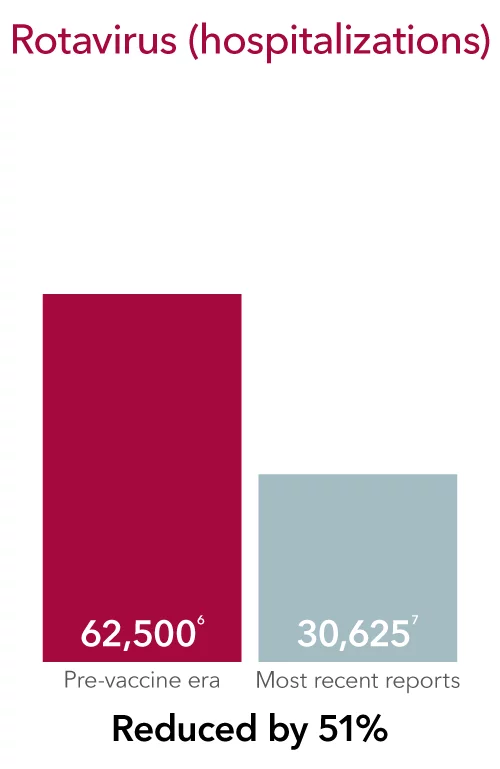
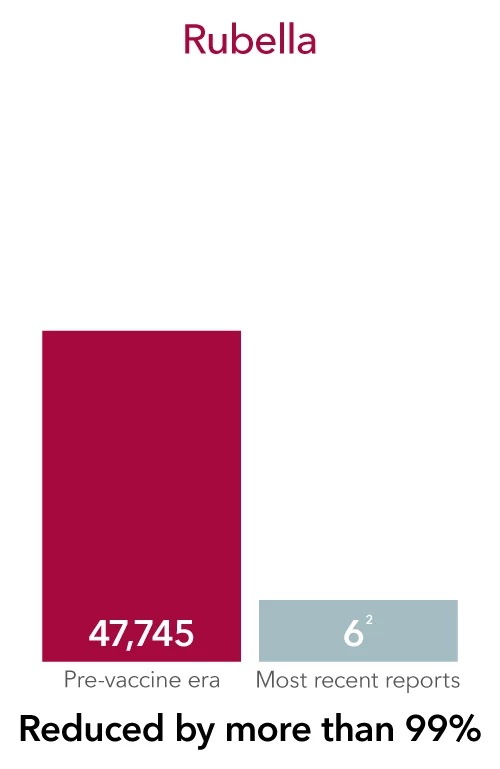
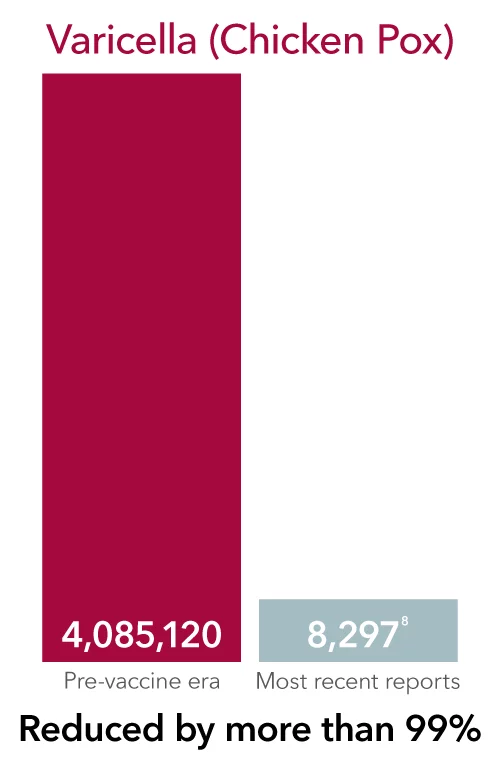
Las vacunas redujeron en gran medida e incluso erradicado muchas enfermedades infecciosas que solían dañar comúnmente, e incluso matar, a personas de todas las edades, en todo el mundo.
Algunas de estas enfermedades todavía existen y puede contraerlas si no está vacunado. De hecho, miles de adultos en los EE. UU. se enferman gravemente y son hospitalizados cada año debido a enfermedades prevenibles por vacunación.
Seguro y conveniente
La vacunación es una de las medidas de atención preventiva más convenientes y seguras disponibles. Es por eso que, durante años, el Departamento de Salud y Servicios Humanos de EE. UU. ha trabajado con socios federales y locales para proteger la salud pública y prevenir enfermedades infecciosas.
Visite a su proveedor de atención primaria para vacunarse y ayudar a protegerse a sí mismo, a su familia y a su comunidad.
Obtenga más información sobre las vacunas más comunes
Vacuna contra la gripe (influenza)
Todas las personas de 6 meses o más deben vacunar contra la gripe cada temporada, especialmente las personas con mayor riesgo de desarrollar complicaciones
Personas en riesgo
Las personas con mayor riesgo de complicaciones graves por la influenza incluyen:
- Adultos de 65 años o más
- Niños menores de 2 años
- Personas menores de 19 años que toman medicamentos que contienen aspirina o salicilato a largo plazo
- Aquellos con un sistema inmunitario debilitado debido a una enfermedad (como las personas con VIH o SIDA, o algunos cánceres como la leucemia) o medicamentos (como los que reciben quimioterapia o radioterapia para el cáncer, o personas con afecciones crónicas que requieren corticosteroides crónicos u otros medicamentos que suprimen el sistema inmunitario).
- Personas con ciertas discapacidades, especialmente aquellas que pueden tener problemas con la función muscular, la función pulmonar o dificultad para toser, tragar o eliminar líquidos de las vías respiratorias.
- Mujeres embarazadas, incluso hasta 2 semanas luego del final del embarazo
- Aquellos que viven en hogares de ancianos y otros centros de atención a largo plazo
- Ciertos grupos minoritarios raciales y étnicos tienen un mayor riesgo de hospitalización por influenza, incluidas las personas negras no hispanas, las personas hispanas o latinas y las personas indígenas americanas o nativas de Alaska.
Condiciones que causan riesgo de complicaciones
Ciertas afecciones y trastornos médicos pueden aumentar el riesgo de complicaciones:
- Asma
- Enfermedad pulmonar crónica (como enfermedad pulmonar obstructiva crónica [EPOC] y fibrosis quística)
- Condiciones neurológicas y del neurodesarrollo
- Trastornos sanguíneos (como anemia de células falciformes)
- Trastornos endocrinos (como diabetes mellitus)
- Enfermedad cardíaca (como cardiopatía congénita, insuficiencia cardíaca congestiva y enfermedad de las arterias coronarias)
- Trastornos renales
- Trastornos hepáticos
- Trastornos metabólicos (como trastornos metabólicos hereditarios y trastornos mitocondriales)
- Índice de masa corporal (IMC) de 40 kg/m2 o superior/Obesidad
- Antecedentes de accidente cerebrovascular
Desde 2010 (excepto la temporada de influenza 2020-2021), se estima que la influenza resultó en 120,000-170,000 hospitalizaciones y 6,300-52,000 muertes en los Estados Unidos. En todo el mundo, la gripe causa entre 290.000 y 650.000 muertes al año.
¿Cuáles son algunos mitos comunes sobre la vacuna contra la gripe?
Vacuna contra el COVID-19
¿Quién debe vacunar contra el COVID-19?
Los niños de 6 meses a 23 meses, los niños y adolescentes de 2 a 18 años y con condiciones de salud que aumentan el riesgo de COVID grave deben vacunar con la vacuna Covid de 2 dosis. Las personas que viven en centros de atención a largo plazo u otros entornos grupales, las personas que nunca fueron vacunadas contra el COVID o las personas que tienen contactos domésticos que tienen un alto riesgo de COVID grave deben vacunar con la vacuna COVID de 2 dosis. Los niños de 2 a 18 años sin factores de riesgo pueden recibir una sola dosis de la vacuna COVID actualizada. La vacuna COVID-19 actualizada o "refuerzo" también se recomienda en cualquier momento durante el embarazo, cuando se planea quedar embarazada, en el periodo posparto o durante la lactancia. Se recomienda una vacuna COVID-19 para todos los adultos, no solo para aquellos con mayor riesgo.
Condiciones que aumentan el riesgo
Ciertas afecciones y trastornos médicos pueden aumentar el riesgo de complicaciones:
- Obesidad
- Afecciones que afectan el sistema inmunitario
- Enfermedad de células falciformes
- Enfermedades cardíacas o afecciones cardíacas congénitas
- Enfermedad pulmonar (incluido el asma)
- Diabetes
- Trastornos del neurodesarrollo como parálisis cerebral
- Enfermedad renal crónica
- Condiciones médicas complejas, incluidas algunas que requieren respiraciones o sondas de alimentación, o ventiladores domésticos
Los adultos mayores de 65 años corren el mayor riesgo de enfermar gravemente de COVID-19. Más del 81% de las muertes por COVID-19 ocurren en personas mayores de 65 años. El número de muertes entre las personas mayores de 65 años es 97 veces mayor que entre las personas de 18 a 29 años. Su riesgo de enfermedad grave por COVID-19 aumenta a medida que aumenta la cantidad de sus afecciones médicas subyacentes. Algunas personas corren un mayor riesgo de enfermar gravemente o morir a causa del COVID-19 debido al lugar donde viven o trabajan, o porque no pueden recibir atención médica. Esto incluye a muchas personas de grupos minoritarios raciales y étnicos y personas con discapacidades.
¿Cuáles son algunos mitos comunes sobre la vacuna COVID19?
Vacuna contra el virus respiratorio sincitial (VRS)
¿Quién debe vacunar contra el VRS?
Todos los adultos de 76 años o más, y los adultos de 50 a 75 años que tienen un mayor riesgo de VRS grave, deben vacunar. Las mujeres que están embarazadas durante la temporada de VRS, o cuyos bebés nacen durante la temporada de VRS, deben recibir una dosis única de la vacuna materna contra el VRS durante las semanas 32 a 36 de embarazo, si esas semanas caen entre septiembre y enero.
Las siguientes afecciones aumentan el riesgo de VRS grave
Ciertas afecciones y trastornos médicos pueden aumentar el riesgo de complicaciones:
- Enfermedad cardiovascular crónica (p. ej., insuficiencia cardíaca, enfermedad de las arterias coronarias o cardiopatía congénita [excluyendo hipertensión aislada]).
- Enfermedad pulmonar o respiratoria crónica (p. ej., enfermedad pulmonar obstructiva crónica, enfisema, asma, enfermedad pulmonar intersticial o fibrosis quística).
- Enfermedad renal en etapa terminal o dependencia de hemodiálisis u otra terapia de reemplazo renal.
- Diabetes mellitus complicada por enfermedad renal crónica, neuropatía, retinopatía u otro daño a órganos diana, o que requiere tratamiento con insulina o inhibidor del cotransportador de sodio-glucosa-2 (SGLT2).
- Afecciones neurológicas o neuromusculares que causan deterioro de la depuración de las vías respiratorias o debilidad de los músculos respiratorios (p. ej., disfagia posterior a un accidente cerebrovascular, esclerosis lateral amiotrófica o distrofia muscular [excluyendo antecedentes de accidente cerebrovascular sin deterioro de la depuración de las vías respiratorias]).
- Enfermedad hepática crónica (por ejemplo, cirrosis).
- Afecciones hematológicas crónicas (p. ej., anemia de células falciformes o talasemia).
- Severe obesity (body mass index ≥40 kg/m2).
- Compromiso inmunológico moderado o grave.
- Residencia en un hogar de ancianos.
- Otras afecciones médicas crónicas o factores de riesgo que un proveedor de atención médica determine que aumentarían el riesgo de enfermedad grave debido a una infección respiratoria viral (p. ej., fragilidad, situaciones en las que los proveedores de atención médica tienen preocupación por la presencia de afecciones médicas crónicas no diagnosticadas, o residencia en una comunidad remota o rural donde el transporte de pacientes con enfermedad grave por VRS para la intensificación de la atención médica es un desafío).
En 2024-2025, el VRS se asoció con 3.6 millones-6.5 millones de visitas ambulatorias por VRS, 190,000-350,000 hospitalizaciones por VRS y 10,000-23,000 muertes por VRS. La vacuna materna contra el VRS redujo el riesgo de que el bebé fuera hospitalizado por VRS en un 68% y el riesgo de tener una visita de atención médica por VRS en un 57% dentro de los 3 meses posteriores al nacimiento. En el mismo ensayo, la vacuna contra el VRS redujo el riesgo de que el bebé fuera hospitalizado por VRS en un 57% y el riesgo de tener una visita de atención médica por VRS en un 51% dentro de los 6 meses posteriores al nacimiento.
¿Cuáles son algunos mitos comunes sobre la vacuna contra el VRS?
MMR: vacuna contra el sarampión, las paperas y la rubéola (sarampión alemán)
¿Quién debe vacunar contra la triple vírica?
Los bebés deben recibir su primera dosis entre los 12 y los 15 meses y la segunda dosis entre los 4 y los 6 años de edad; todos los adultos deben tener 2 dosis documentadas de MMR o tener documentación de títulos que muestren protección.
Antes de que comenzara el programa de vacunación contra el sarampión en 1963, se estima que entre 3 y 4 millones de personas en los EE. UU. contrajeron sarampión y 48,000 personas fueron hospitalizadas con 500 muertes por año. Hay brotes continuos de sarampión en los EE. UU., Canadá, México y el mundo, lo que aumenta el riesgo de infección en personas no inmunizadas. La infección por el virus de las paperas puede causar inflamación en los testículos o los ovarios, lo que puede conducir a la infertilidad permanente. También puede causar sordera, inflamación del páncreas e inflamación del cerebro. La infección por rubéola durante el embarazo puede causar un aborto espontáneo o muerte fetal. El síndrome de rubéola congénita, que puede causar retrasos en el crecimiento, cataratas, sordera, defectos cardíacos congénitos y problemas de aprendizaje, ocurre en hasta el 85% de los bebés nacidos de personas que tuvieron rubéola en las primeras 12 semanas de embarazo.
¿Cuáles son algunos mitos comunes sobre la vacuna MMR?
Vacuna contra la varicela
¿Quién debe vacunar contra la varicela?
Los bebés deben recibir su primera dosis entre los 12 y los 15 meses y la segunda dosis entre los 4 y los 6 años de edad. Las personas de 13 años o más deben recibir dos dosis con un intervalo de 4 a 8 semanas sin evidencia de inmunidad (si pasaron más de 8 semanas desde la primera dosis, la segunda dosis se puede gestionar sin resetear el serial). La vacuna también se recomienda para grupos específicos si no tienen evidencia de inmunidad, incluidas las personas con infección por VIH, las personas con algún grado de inmunodeficiencia, los contactos domésticos de personas inmunodeprimidas, las madres posparto y lactantes y el personal de atención médica.
La "varicela" solía infectar a 4 millones de personas en los Estados Unidos cada año. Más de 10,000 fueron hospitalizados y más de 100 murieron. Un caso leve puede hacer que un niño falte a la escuela o a la guardería durante una semana o más.
¿Cuáles son algunos mitos comunes sobre la vacuna contra la varicela?
Vacuna contra el herpes zóster (culebrilla)
¿Quién debe recibir la vacuna contra el herpes zóster?
Los adultos de 50 años o más deben recibir 2 dosis de vacuna separadas por 2 a 6 meses. Cualquier persona de 19 años o más con un sistema inmunitario debilitado también debe recibir la vacuna.
Aproximadamente 1 de cada 3 personas en los Estados Unidos tendrá herpes zóster en su vida y el riesgo de herpes zóster aumenta con la edad. El herpes zóster causa una erupción dolorosa y puede complicar con neuralgia postherpética (NPH), un dolor nervioso a largo plazo que puede ser severo y debilitante. El dolor ocurre en las áreas donde estaba la erupción del herpes zóster. La NPH puede durar meses o años después de que desaparece la erupción.
¿Cuáles son algunos mitos comunes sobre la vacuna contra el herpes zóster?
Vacuna contra la hepatitis B
¿Quién debe recibir la vacuna contra la hepatitis B?
Los niños deben recibir su primera dosis dentro de las 24 horas posteriores al nacimiento. Pueden recibir su 2ª dosis de 4 a 8 semanas luego de la 1ª dosis, y su 3ª dosis aproximadamente 6 meses después y al menos 4 meses luego de la primera dosis. Los niños y adolescentes de 7 a 18 años pueden recibir su 1.ª dosis en cualquier momento, su segunda dosis 4 semanas después y su 3.ª dosis 38 semanas después y al menos 16 semanas luego de la primera dosis. Mayores de 19 años: 2, 3 o 4 dosis según la vacuna específica empleada y las indicaciones.
Alrededor de 260 millones de personas viven con hepatitis B crónica. Esto significa que aproximadamente 1 de cada 32 personas en todo el mundo vive con una infección crónica por hepatitis B. La hepatitis B es 100 veces más infecciosa que el VIH. Las personas contraen con mayor frecuencia hepatitis B por contacto con la sangre. La sangre de una persona infectada con el virus de la hepatitis B está muy contaminada con el virus. El virus está presente en niveles tan altos que puede propagar por contacto con cantidades de sangre demasiado pequeñas para ver. El virus también puede sobrevivir en superficies más tiempo que la mayoría de los virus, hasta siete días. Como resultado, incluso el contacto casual con la sangre de alguien infectado puede causar infección. El contacto casual puede incluir compartir paños, cepillos de dientes o maquinillas de afeitar. El virus también puede propagar entre los miembros del equipo, particularmente para los deportes de contacto donde la exposición a la sangre es más común. También se sabe que las personas contraen hepatitis B por tatuajes y equipos médicos contaminados. Las personas más propensas a entrar en contacto con la sangre de las personas infectadas tienen un mayor riesgo de contraer hepatitis B. Esto incluye a los trabajadores de la salud, los usuarios de drogas intravenosas y los recién nacidos de madres infectadas con el virus. Las personas también pueden infectar a través del contacto sexual. El virus está presente en el semen y los fluidos vaginales.
¿Cuáles son algunos mitos comunes sobre la vacuna contra la hepatitis B?
Vacuna contra el virus del papiloma humano (VPH)
¿Quién debe recibir la vacuna contra el VPH?
La edad mínima para la vacuna contra el VPH es de 9 años. Se recomienda comenzar entre los 9 y los 12 años y poner al día con la vacunación para todos aquellos que no estén completamente vacunados a los 18 años. Si es menor de 15 años, es un serial de 2 dosis con un intervalo de 6 a 12 meses. Si tiene más de 15 años, es un serial de 3 dosis: dosis 1, luego dosis 2: 1-2 meses después y dosis 3: 6 meses luego de la 1ª dosis. Recomendado para adultos de 19 a 26 años y puede ser una consideración para adultos de 27 a 45 años, pero recomendaría hablar con el proveedor.
La vacuna contra el VPH protege contra la infección por el virus del papiloma humano (VPH), que puede provocar ciertos cánceres y verrugas genitales. Es una forma altamente efectiva de prevenir más del 90% de los cánceres de cuello uterino, vagina, vulva, pene, ano y garganta, así como verrugas genitales.
¿Cuáles son algunos mitos comunes sobre la vacuna contra el VPH?
Necesita vacunas durante toda su vida
Debe asegurarse de que sus vacunas estén al día porque la inmunidad puede desaparecer a medida que envejece y corre el riesgo de contraer diferentes enfermedades en la edad adulta. Los Centros para el Control y la Prevención de Enfermedades (CDC, por sus siglas en inglés) recomiendan que todos los adultos se vacunen para ayudarlos a prevenir contraer y propagar enfermedades graves que podrían resultar en mala salud, faltas al trabajo, facturas médicas y no poder cuidar a la familia.
Tu médico de cabecera hablará contigo sobre el calendario de vacunación según tu edad y condición, así como para tus hijos. Infórmate más sobre las vacunas infantiles y los calendarios recomendados.
Recomendaciones de los CDC para adultos
Según los CDC, todos los adultos:
- Necesita vacunarse contra la gripe estacional (influenza) todos los años. La vacuna contra la influenza es especialmente importante para las personas con afecciones crónicas, las mujeres embarazadas y los adultos mayores.
- Deben recibir la vacuna Tdap una vez si no la recibieron en la adolescencia para protegerse contra la tos ferina (tos ferina), y luego una vacuna de refuerzo Td (tétanos, difteria) cada 10 años. Además, las mujeres deben recibir la vacuna Tdap cada vez que estén embarazadas, preferiblemente entre las semanas 27 y 36. Además, los CDC recomiendan la vacunación contra el tétanos para todos los bebés y niños, preadolescentes, adolescentes y adultos.
Otras vacunas a tener en cuenta
Además, es posible que necesite otras vacunas según su edad, condiciones de salud, trabajo, estilo de vida o viajes. Las siguientes enfermedades se pueden prevenir siguiendo las pautas de los CDC para las vacunas:
- Difteria. Una enfermedad grave causada por una toxina producida por bacterias. Puede dañar el corazón, los pulmones y los nervios. Puede ser fatal.
- Haemophilus influenzae tipo b (Hib). Infección bacteriana que provoca afecciones graves como meningitis, neumonía y epiglotitis.
- Hepatitis A. Enfermedad viral del hígado. Puede contraerse al comer alimentos o beber agua contaminada con heces, o puede contraerla al entrar en contacto con alguien que tenga la infección.
- Meningitis meningocócica. Infección bacteriana grave de las membranas que cubren el cerebro y la médula espinal (meninges) y que puede poner en peligro la vida.
- Neumonía neumocócica. Infección pulmonar grave causada por la bacteria Streptococcus pneumoniae.
- Poliomielitis. Una enfermedad viral altamente infecciosa que afecta el sistema nervioso y puede provocar parálisis permanente. La poliomielitis fue casi completamente erradicada gracias a las vacunas
- Rotavirus. Un virus altamente contagioso que es la principal causa de diarrea grave en los niños.
- Tos ferina (tos ferina). Una enfermedad respiratoria altamente contagiosa que puede provocar convulsiones, lesiones cerebrales y la muerte en bebés pequeños.
Efectos secundarios de las vacunas
En la mayoría de los casos, las vacunas se administran a través de una inyección, por lo que los efectos secundarios más comunes son dolor leve, enrojecimiento o hinchazón en el lugar de la inyección, que desaparecen en unos pocos días.
Los efectos secundarios graves son muy raros. Su proveedor de atención primaria analizará con usted los posibles efectos secundarios para ayudarlo a decidir qué es lo mejor para usted y su familia.
Las últimas noticias en vacunas
Bibliografía
Centro para el Control y la Prevención de Enfermedades (CDC). Calendarios de vacunación – https://www.cdc.gov/vaccines/schedules/index.html
Organización Mundial de la Salud (OMS). Vacunas e inmunización – https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1
Nota a pie de página:
- CDC. JAMA 14 de noviembre de 2007; 298(18): 2155–63.
- CDC. Enfermedades y afecciones infecciosas de notificación obligatoria a nivel nacional, Estados Unidos: Tablas anuales 2019. Consultado el 2 de agosto de 2022.
- CDC. Vigilancia de la hepatitis viral - Estados Unidos, 2019. Publicado en mayo de 2021. El total estimado de casos explica el subregistro.
- CDC. MMWR 6 de octubre de 1995; 43(53):1–98.
- CDC. Reporte de vigilancia bacteriana activa del núcleo (ABC); Red del Programa de Infecciones Emergentes Streptococcus pneumoniae, 2019.
- MMWR, 6 de febrero de 2009; 58 (RR-2): 1–25.
- CDC. New Vaccine Surveillance Network, datos de 2017 (no publicados); La enfermedad por rotavirus en los Estados Unidos ahora tiene un patrón bienal.
- CDC. Programa de varicela, datos de 2017 (no publicados)





